 In my earlier article about oxalates, I explained how oxalates influence the biochemical progression and symptomatic expression of varied chronic diseases. Through an overarching “lens” of 15 years’ research and clinical experience with autism, I identified multiple areas for scientific inquiry and therapeutic direction for a variety of chronic health conditions and underlying symptomatology.
In my earlier article about oxalates, I explained how oxalates influence the biochemical progression and symptomatic expression of varied chronic diseases. Through an overarching “lens” of 15 years’ research and clinical experience with autism, I identified multiple areas for scientific inquiry and therapeutic direction for a variety of chronic health conditions and underlying symptomatology.
This article specifically investigates oxalates and autism; where the range of metabolic implications is vast – from impairment of mitochondrial function (and energy production) to disruption of mineral balance and the creation of severe oxidative stress in the body. The down stream effects of these biochemical aberrations touch dozens of systemic avenues.
I’ll explain some of the processes that can be severely affected in autism, that are likewise noted in those with oxalate impairment, and explore the potential role of high oxalate in the body as a pathogenesis (biological mechanism or cause) of autism. These symptomatic expressions, and the findings from several key studies highlighted in this article, prompt eager investigation of the role of oxalates in autism.
Before we begin, to understand the basics: what oxalate is, where it comes from, and common symptoms read my previous article on oxalate.
Oxalates in Autism Study
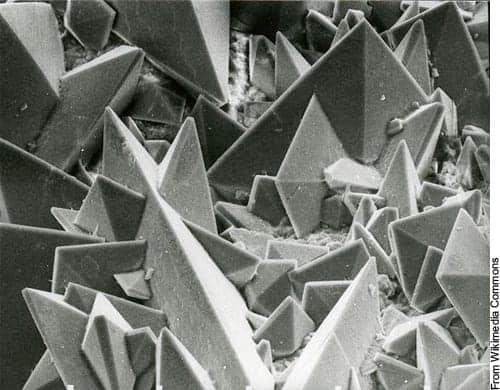
 In 2012, the European Journal of Paediatric Neurology published a study that investigated the role of oxalates in autism. Researchers measured a 2.5-fold greater level of oxalates in the urine, and a three-fold greater level of oxalate in the plasma, in children with autism.1
In 2012, the European Journal of Paediatric Neurology published a study that investigated the role of oxalates in autism. Researchers measured a 2.5-fold greater level of oxalates in the urine, and a three-fold greater level of oxalate in the plasma, in children with autism.1
Their finding was specifically, hyperoxaluria; a condition of high oxalate. Interestingly though, high oxalate levels in urine did not necessarily correlate with high levels in the plasma. One child might have high urinary levels, but not high plasma; another might have high plasma levels, but not high urine.
A clinical challenge we face today is that only urinary levels are being used as an indicator of oxalate levels.
Plasma oxalate testing is only available in a research setting. The 2012 study tells us that not every child with oxalate impairment will present with high oxalate in their urine (they might have high oxalate in their plasma). This makes determining high oxalate, via testing (urine only), very challenging.
It’s significant to note that the study on autism and oxalate excluded the following groups from their selection criteria: those on a special diet, those with a history of seizures or antibiotic use, those with gastrointestinal disease (in addition to those with kidney stones). This is important to note, because all of these can be conditions of or cause hyperoxaluria.
Also noteworthy is a chart representing all of the controls (you can look at the study online here) on the top of page 5. You’ll notice all the controls have little blue boxes. There’s almost an invisible line at 0.05, and all of the controls fit within that 0.05 level. But the autism subjects were all over the map. Apparently, healthy controls are able to regulate the oxalate much better than other people (in this study, people with autism).
A history of antibiotic use can make oxalate issues worse, as can gastrointestinal diseases. Clinicians report that children with autism have higher rates of antibiotic use and seem less able to fight infection, and research demonstrates that gastrointestinal conditions are higher in autism than for neurotypical children.[4],[5],[6] Also, many autistic children suffer seizures, and oxalates can cause seizures.[7],[8],[9]
The study’s selection criteria (omissions) may affect an underrepresentation of the range of oxalate (plasma and urinary) that would occur in a full range of autistic patients. Even with the exclusions, significant oxalate issues were identified. This warrants further study, without excluded variables, to investigate how results may differ. If these groups had been included, rates and levels of oxalate would most likely be even higher.
Interestingly, the researchers had expert oxalate scientists review their findings, specifically the 2.5 – 3-fold increase in oxalate levels. The scientists were concerned for the children’s health. The levels were so high that they felt the children should (and may) have serious health implications based on oxalates in this elevated range; they’ve witnessed the detrimental effects of oxalate levels that high.
In summary, the study concluded that: “hyperoxalemia or hyperoxaluria may be involved in the pathology of autism spectrum disorders in children.” 1 It then continues to explain that based on the high oxalate finding, certain treatment options, such as a low oxalate diet, probiotic therapy, possibly with Oxalobacter formigenes, and a variety of supplementation may be helpful in these children.1
Oxalates are significant in autism because clinically we see a great deal of oxidative stress, considerable inflammation, mitochondrial damage or dysfunction, as well as faulty sulfation and seizures—areas where oxalates can wreck havoc. The discovery and clear indication that high oxalate may be involved in the pathology of autism is both significant and hopeful. This research and the biochemical connections we are highlighting provide further hope and direction for helping children with autism.
How Oxalates Cause Problems in Autism
 I’ll next explain some of the systemic processes that can be severely affected in those with autism, that are likewise noted in those with oxalate problems – then I’ll explore the link between the two, and the possibility of high oxalates as a pathogenesis of autism.
I’ll next explain some of the systemic processes that can be severely affected in those with autism, that are likewise noted in those with oxalate problems – then I’ll explore the link between the two, and the possibility of high oxalates as a pathogenesis of autism.
Firstly, let’s discuss how the health (or dis-ease) in the gut and certain nutrient deficiencies affect whether someone is more susceptible to a condition of high oxalate. And then let’s explore how oxalates can cause or exacerbate the conditions often found in autism:
- Oxidative stress
- Inflammation
- Mitochondrial damage[10]
- Seizures7,8,9
- Faulty sulfation
Gastrointestinal Tract
As noted in my earlier article, the health of the gastrointestinal tract influences whether someone develops a problem with oxalates. Leaky gut, insufficient beneficial bacteria (including but not limited to a species called Oxalobacter Formigenes), poor fat digestion, and insufficient mineral intake affect whether (and how much) oxalate gets absorbed into the bloodstream from the gut. Many of these conditions, particularly leaky gut and a poor microbial balance, are common in those with autism.
Gut issues are so prevalent in autism,[11] and this condition in the gut compounds the potential problems with oxalate, and makes issues with oxalate more likely.
Compromised digestive capacity and an impaired ability to metabolize oxalate compounds may be linked to complications in autism. According to autism advocate and activist Dr. Leigh Ann Chapman, “Ordinarily, not much oxalate is absorbed from the diet, but the level of absorption has to do with the condition of the gut. There is a lot of medical literature showing that when the gut is inflamed, when there is poor fat digestion (steatorrhea), when there is a leaky gut, or when there is prolonged diarrhea or constipation, excess oxalate from foods that are eaten can be absorbed from the GI tract and become a risk to other cells in the body. Since these gastrointestinal conditions are found frequently in autism, it seems reasonable to see if lowering the dietary supply of oxalates could be beneficial.” [12]
Nutrient Deficiencies and Endogenous Production
Each person’s ability to process oxalate varies, based on the health of their gut as mentioned above, as well as nutrient deficiencies, systemic conditions, and genetic differences. Some deficiencies, including vitamin B6 and B1 deficiency can cause the body to produce oxalate (endogenously) in problematic amounts. This means that in children deficient in these important B vitamins, their body can create oxalate, rather than requiring it to come in from the diet. B6 deficiency is very common in autism, and for decades studies have shown the benefits of B6 supplementation in autism. Other deficiencies such as vitamin A deficiency can cause the body to absorb excess oxalate through the gut.
Further, because one’s body chemistry can convert a substance into oxalate; such as supplements like ascorbic acid or the amino acid glycine (a key component in bone broth) – complications can arise. Fructose, xylitol, and other sugar alcohols can also convert to oxalate. Certain supplements, as well as a diet too high in meat, can be a problem for some people.
In addition to oxalate levels increasing with nutrient deficiency, oxalates themselves can cause nutrient deficiency. When oxalate is present from the diet, oxalate in the gut binds to minerals and inhibits absorption. This means diets high in oxalate can cause mineral deficiency including calcium and magnesium deficiency.
Oxidative Stress and Inflammation
Oxalates can lead to oxidative stress, and subsequently cause inflammation and injury.[13], [14] Because high oxalates can elevate superoxide (i.e. free radicals), they deplete glutathione and antioxidant status.[15]
Oxidative stress, inflammation, and low glutathione status are common occurrences in autism[16], [17], as well as many other chronic diseases. By understanding this relationship and recognizing a potential source of chronic inflammation and stress, practitioners can better address what may be causing the problems. And in this case, oxalate is an important factor to consider.
Mitochondrial Damage
Oxalates can also damage mitochondria. In the 2008 Veena study, researchers concluded that mitochondrial damage is an essential event in hyperoxaluria, so when you have high oxalates, you will have damage to the mitochondria. The same study indicated that oxalate impairs mitochondrial function. They found high oxalate created 30% depression of Complex I, a 54% depression of Complex II, a 35% depression of Complex III, and a 63% depression of Complex IV.12
Further, mitochondrial dysfunction has been found in autism.14, [18] Oxalates decrease mitochondrial function and increase oxidative stress, which is really important to consider for the many different conditions that can seriously affect the mitochondria, including autism.
Seizures
Twenty-two to thirty percent of children with autism suffer seizures.[19], [20] It is also postulated that one cause for these seizures may be neuro-inflammation.[21] We know that oxalates can cause seizures and also create inflammation. Therefore it is quite possible that oxalates may be a cause of seizures in autism.
Interestingly, the fruit carambola (also known as starfruit) is popular throughout Southeast Asia and the South Pacific and contains a high amount of oxalate. One study noted that “Carambola contains a large quantity of oxalate, which can induce depression of cerebral function and seizures.” 9
Studies have shown that high oxalate levels can cause seizures in individuals. Specifically, people with high oxalate whether from poisoning from accidental ingestion or antifreeze, or in other cases due to liver or kidney transplants, what the researchers found in essence was that oxalate can cause seizures.
As noted in the Oxalates and Autism study, the researchers did not “count” people that were on a special diet or those with a history of seizures. And, as explained earlier, seizures can stem from a condition of high oxalate. Again, it would be useful to repeat this study and include people with seizures, to see if prevalence of oxalate issues in autism is even higher than initially measured – and if oxalates may play a role in the etiology of seizures or exacerbate seizures.
Sulfur and Poor Sulfation
It’s equally important to understand sufate and sulfation when investigating autism and oxalates.
The body requires sulfate for vital sulfation processes, including processing phenolic foods. If certain foods or substances are consumed (or even inhaled) when sulfate is low, it can cause phenol reactions such as red cheeks and ears, hyperactivity, irritability, aggression, sleep issues, and more. There is much literature about poor sulfation and autism; I see these noted reactions often in my nutrition practice. Therefore, some children and adults with autism that have low sulfate often also have an issue with phenols and with oxalates. Not always, but these biochemical relationships suggest that some children may find relief by avoiding both for a period of time.
In regard to oxalate, when sulfate is low, oxalate can get into the cell on the sulfate transporter and interfere with cellular function.
There is a two-way relationship with oxalate and sulfate. Not only can oxalates lead to poor sulfation (as mentioned above) oxalate can also interfere with the body’s ability to allow sulfate into the cell inhibiting sulfation. And as mentioned above, low sulfate levels can allow oxalate into the cell on the (unoccupied) sulfate transporter. When this happens, it can affect the mitochondria and subsequently virtually every system of the body.
In autism, there seems to be a vicious ATP/sulfate challenge that we see. We often find high sulfate in the urine, and this gives some practitioners the false notion that sulfate is sufficient, if not high. However, while it’s high in the urine, we often find low sulfate and poor sulfation in autism. Why is this?
My hypothesis: oxalates could be at play. If ATP is low, the kidneys need ATP to recycle sulfate and, with low ATP, it could cause sulfate to be low. If sulfate is low, it allows oxalate to get into the cell, and it can decrease ATP production. When ATP is low, it can lead to low sulfate, both because it can decrease SAMe going through that pathway, as well as low ATP in the kidneys, causing the dumping of sulfate (causing it to be high in the urine when the body desperately needs it).
Either way, regardless of the cause of low sulfate, children with autism are known to have low sulfate and poor sulfation.[22],[23],[24] Therefore addressing high oxalates and low sulfate when they are an issue can be very helpful to children with autism.
Conclusion
Oxalates are a promising and emerging field that far exceeds kidney stone issues. Investigating their effects on the mitochondria, inflammation, and all systems of the body, reveals that oxalates play a role in many chronic diseases. The study “A potential pathogenic role of oxalate in autism” revealed hyperoxaluria in autism, further helping define the role of oxalate in autism.
With autism, oxalates can cause oxidative stress, inflammation, and seizures; something that is corroborated by the actual prevalence of these conditions in those with autism. Moreover, the conditions under which oxalates can become most problematic: disrupted microbiome, leaky gut, poor sulfation, B6 deficiency, and diets high in oxalate, are also common in autism.
I’ve been researching the influence of oxalates and utilizing a low oxalate diet for more that a dozen years. My future articles on this subject with explain: high oxalate foods, low oxalate diets, and important supplement support. Most importantly, I’ll provide best practices for implementing a low oxalate diet; how to decrease oxalates in food, know when it’s enough, and other ways to support the body during this process. Sometimes one key clinical insight can “course correct” someone’s existing diet and lead to new breakthroughs; often, it’s oxalates.
It’s critical that, as practitioners and professionals, we look at the role of oxalates in autism, so we can encourage further research and best support our patients, clients, and families in need.
IMPORTANT POINT: It’s very common when people first learn about oxalates and feel this might apply to them that they often attempt to remove them right away, but I strongly caution against removing oxalates quickly. It can cause pain, discomfort and problems when you remove oxalates quickly. It’s best to learn about them first or get help from a qualified nutrition professional.
Learn More on Oxalates
Join my Nourishing Hope for Healing Kids, nutrition program for parents and individuals, to learn more about oxalates, and how to personalize diet and nutrition to help improve autism and other neurological conditions.
Scientific References:
 [1] Konstantynowicz, J., Porowski, T., Zoch-Zwierz, W., Wasilewska, J., Kadziela-Olech, H., Kulak, W., Owens S.C., Piotrowska-Jastrzebska J., and Kaczmarski, M. (2012). A potential pathogenic role of oxalate in autism. European Journal of Paediatric Neurology, 16(5), 485-491.
[1] Konstantynowicz, J., Porowski, T., Zoch-Zwierz, W., Wasilewska, J., Kadziela-Olech, H., Kulak, W., Owens S.C., Piotrowska-Jastrzebska J., and Kaczmarski, M. (2012). A potential pathogenic role of oxalate in autism. European Journal of Paediatric Neurology, 16(5), 485-491.
[2] Terribile, Maurizio, Maria Capuano, Giovanni Cangiano, Vincenzo Carnovale, Pietro Ferrara, Michele Petrarulo, and Martino Marangella. “Factors increasing the risk for stone formation in adult patients with cystic fibrosis.” Nephrology Dialysis Transplantation 21, no. 7 (2006): 1870-1875.
[3] Danese, Silvio, Stefano Semeraro, Alfredo Papa, Italia Roberto, Franco Scaldaferri, Giuseppe Fedeli, Giovanni Gasbarrini, and Antonio Gasbarrini. “Extraintestinal manifestations in inflammatory bowel disease.” World Journal of Gastroenterology 11, no. 46 (2005): 7227.
[4] Molloy CA, Manning-Courtney P: Prevalence of chronic gastrointestinal symptoms in children with autism and autistic spectrum disorders. Autism 2003, 7(2):165-171.
[5] Nikolov Roumen N, Bearss Karen E, Jelle Lettinga, Craig Erickson, Maria Rodowski, Aman Michael G, McCracken James T, McDougle Christopher J, Elaine Tierney, Benedetto Vitiello, Eugene Larnold, Bhavik Shah, Posey David J, Louise Ritz, Lawrence Scahill: Gastrointestinal Symptoms in a Sample of Children with Pervasive Developmental Disorders. J Autism Dev Disord 2009, 39:405-413.
[6] Adams, J. B., Johansen, L. J., Powell, L. D., Quig, D., & Rubin, R. A. (2011). Gastrointestinal flora and gastrointestinal status in children with autism–comparisons to typical children and correlation with autism severity. BMC gastroenterology, 11(1), 22.
[7] Díaz, Cándido, et al. “Long Daily Hemodialysis Sessions Correct Systemic Complications of Oxalosis Prior to Combined Liver–Kidney Transplantation: Case Report.” Therapeutic Apheresis and Dialysis 8.1 (2004): 52-55.
[9] Chen, Chien-Liang, et al. “Neurotoxic effects of carambola in rats: the role of oxalate.” Journal of the Formosan Medical Association 101.5 (2002): 337-341.
[10] Veena, C. K., Josephine, A., Preetha, S. P., Rajesh, N. G., & Varalakshmi, P. (2008). Mitochondrial dysfunction in an animal model of hyperoxaluria: a prophylactic approach with fucoidan. European journal of pharmacology, 579(1), 330-336.
[11] McElhanon, Barbara O., Courtney McCracken, Saul Karpen, and William G. Sharp. “Gastrointestinal Symptoms in Autism Spectrum Disorder: A Meta-analysis.” Pediatrics 133, no. 5 (2014): 872-883.
[12] Chapman, L. A. (2007). A Low Oxalate Diet for Autism. Retrieved December 1, 2015, from www.http://chapmannd.com
[13] Biswas, Subrata K., et al. “Which comes first: renal inflammation or oxidative stress in spontaneously hypertensive rats?.” Free radical research 41.2 (2007): 216-224.
[14] Khan, Saeed R. “Hyperoxaluria-induced oxidative stress and antioxidants for renal protection.” Urological research 33.5 (2005): 349-357.
[16] Rose, S., S. Melnyk, O. Pavliv, S. Bai, T. G. Nick, R. E. Frye, and S. J. James. “Evidence of oxidative damage and inflammation associated with low glutathione redox status in the autism brain.” Translational psychiatry 2, no. 7 (2012): e134.
[17] Rossignol, D. A., and R. E. Frye. “A review of research trends in physiological abnormalities in autism spectrum disorders: immune dysregulation, inflammation, oxidative stress, mitochondrial dysfunction and environmental toxicant exposures.” Molecular psychiatry 17.4 (2011): 389-401.
[18] Rossignol, D. A., and R. E. Frye. “Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis.” Molecular psychiatry 17, no. 3 (2011): 290-314.
[19] Volkmar FR, Nelson DS: Seizure disorders in autism. J Am Acad Child Adolesc Psychiatry 1990, 29:127-129.
[20] Tuchman R, Rapin I: Epilepsy in autism. Lancet Neurol 2002, 1:352-358.
[21] Theoharides, Theoharis C., and Bodi Zhang. “Neuro-inflammation, blood-brain barrier, seizures and autism.” J Neuroinflammation 8.1 (2011): 168.
[22] Waring, R. H., and L. V. Klovrza. “Sulphur metabolism in autism.” Journal of Nutritional and Environmental Medicine 10, no. 1 (2000): 25-32.
[23] Alberti, Antonino, Patrizia Pirrone, Maurizio Elia, Rosemary H. Waring, and Corrado Romano. “Sulphation deficit in “low-functioning” autistic children: a pilot study.” Biological psychiatry 46, no. 3 (1999): 420-424
[24] Waring, R. H., Ngong, J. M., Klovrza, L., Green, S., & Sharp, H. (1997). “Biochemical parameters in autistic children.” Developmental Brain Dysfunction, 10, 40-43.





I meant sulfite to sulfate.
Recommended by Dr. Daisy Tran.
My 10 year old son is in the severe part of the spectrum, non verbal, sensory processing disorder, weak fine motor skills, overweight, bad eating habits and demonstrates self injurious behavior. Seeking help.
Hi there Jenna,
Were you considering joining the Nourishing Hope program? https://nourishinghope.com/program/ or perhaps seeking a nutrition practitioner for support. If the latter, please send an email to appointments@nourishinghope.com to receive information and resources.
Thank you!
Hi,
I’m wondering if you can also tell hyperoxolatesfrom looking at stool? My 2 year old has very sandy stool and I am worried about oxolates. She is otherwise very healthy, never had antibiotics and had a delayed, spread out vaccine schedule. Is not autistic.
Hi Esra, Sandy stools are something that some people on the oxalate groups report as relatively common with high oxalates. It’s not definitive that it’s oxalate as I don’t believe the “sand” has ever been tested. But it happens to be a finding among some people with high oxalates. It might be something to consider and discuss with your health practitioner if you feel there might be areas to address.
I’m wondering if oxalates can cause problems for me if they’re not building up in my system. I had a OAT test a few months ago and they were low to normal for the 3 different markers. Thanks!
Hi Linda, everyone eats some oxalates, some much or than others. Oxalates can still inhibit minerals from absorbing through the gut if they are high in the diet, whether they absorb and “build up” (as you say) or not. And some people (as you saw from the article above) create oxalate inside their bodies. When they in the blood stream and get into the cells, they can cause a host of other problems. The OAT test is only one way of assessing an oxalate issue. Unfortunately, plasma levels cannot be tested at this point. OAT is a good place to start, but if you suspect oxalate issues for other reasons, you may want to dig further with your healthcare provider.
Dr Greg Nigh has a summit sulfation problems with IBS. I think he said that glutamine will be converted to glutamate when the person doesn’t have enough sulfate. Glutamate makes people feel irritable, and so it doesn’t help you until you fix the sulfation pathway. The problem is conversion of sulfate to sulfate; the and we is to get sulfate to your extremities. If you haven’t listened to his podcast, perhaps he is suggesting a way to fix this problem. (Epsom salts baths, molybdenim to support sulfation, capsacin, and temporary low sulfur diet to drain the body of its backup of sulfur). It’s something to consider.
I think improving sulfation when possible is generally a good idea. In my programs: for parents, Nourishing Hope for Healing Kids and for practitioners, BioIndividual Nutrition, I often talk about the important of trying to improve the underlying biochemistry and factors that can influence not only nutrition but food intolerances and food reactions. Sometimes this can support a more well rounded diet. Thanks for sharing Dr. Greg Nigh’s information. I have heard him talk about sulfate.